The retina is a vital component of the eye, playing a crucial role in our vision. As a thin layer of tissue near the optic nerve at the back of the eye, the retina acts as a powerful sensory receptor. It converts light focused on it by the eye’s lens into electrical signals, which are then transmitted to the brain.
The retina enables us to perceive colors, differentiate between light intensities, and perform essential daily tasks such as reading and driving. Its photoreceptor cells and optic nerve communicate visual information to the brain.
However, damage to the retina can lead to vision loss and even blindness. Therefore, it is crucial to address retinal conditions promptly to protect and preserve your eyesight.
Some of the commonly encountered retinal conditions include:
- Age-related macular degeneration:
- Retinal detachment
- Diabetic-related eye conditions: Individuals with diabetes are at risk of developing retinopathy, a condition that damages the blood vessels in the retina. If left untreated, diabetic retinopathy can lead to vision impairment.
- Macular hole: A macular hole is a small break in the macula, the central part of the retina responsible for sharp, detailed vision. Surgical intervention may be necessary to restore vision in severe cases.
- Floaters: Floaters are specks or cobweb-like shapes that appear to drift across your field of vision. While they are usually harmless, sudden changes in the number or size of floaters may indicate a retinal issue that requires attention.
If you experience any symptoms such as sudden vision changes, flashes of light, or the appearance of new floaters, it is crucial to consult a retina specialist. Early detection and appropriate treatment can significantly improve outcomes for retinal conditions.
At Roya Eye Clinic, our retina specialists employ state-of-the-art diagnostic tools and advanced treatment techniques to preserve and restore your precious eyesight.
Conditions & treatment
Diabetic Retinopathy
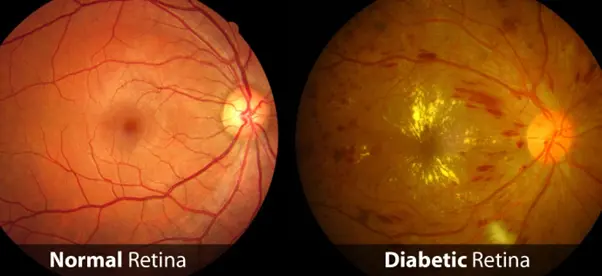
Diabetic retinopathy is a complication of uncontrolled diabetes and consistently high blood sugar over several years, leading to retinal disease. This condition can interfere with the retina’s ability to transmit images to the brain through the optic nerve.
Blood vessels in the retina play a crucial role in supplying it with oxygen and nutrients, keeping it healthy and functioning effectively.
Diabetic retinopathy can cause damage to the blood vessels in the retina, leading to bleeding, leakage, or blockages that result in cell damage within the retina itself.
There are varying forms and levels of severity of diabetic retinopathy. For instance, when the retina is damaged, new blood vessels may grow on it, which can burst and cause bleeding, leading to blurred vision. If the macula, the central area of the retina, is affected, this is known as diabetic maculopathy, indicating a more advanced and serious stage of the disease.
High blood pressure combined with diabetes leads to an even more dangerous condition.
Treatment
Different treatment options are available for diabetic retinopathy, and sometimes a combination of these treatments is used. These include intravitreal injections of medications such as anti-VEGF agents and steroids, conventional peripheral laser treatment, and subthreshold micro-pulse laser therapy. In more advanced cases, particularly with proliferative retinopathy or significant intravitreal haemorrhages, surgery may be necessary as the only viable option.
Early diagnosis of diabetes-related complications, including diabetic retinopathy, generally leads to better management and outcomes. Regular eye screenings are therefore vitally important to detect and manage these conditions promptly.
Age-related Macular Degeneration (AMD)

The central part of the retina, known as the macula, is crucial for controlling the quality and sharpness of our central vision. Macular degeneration is a condition that affects the macula, often resulting in distortion or sometimes loss of central vision (while peripheral vision remains intact). This can significantly impact everyday tasks such as reading and driving. The good news is that the deterioration of vision in macular degeneration typically occurs slowly over time.
There are two main types of macular degeneration: ‘wet’ and ‘dry’. The ‘wet’ form involves the growth of abnormal blood vessels under the macula, which can lead to sudden and severe loss of central vision. This constitutes a medical emergency, requiring urgent treatment to prevent further vision loss.
Treatment
Intravitreal injections are used for treating wet age-related macular degeneration (AMD) by delivering anti-VEGF medications directly into the eye. Regular injections of anti-VEGF drugs can effectively halt the growth, leakage, and bleeding of abnormal blood vessels under the retina, which are characteristic of wet AMD. Most individuals with wet AMD require multiple injections throughout the year, necessitating convenient access to care.
While laser treatment is an option for specific forms of AMD, it is generally less effective for most cases compared to anti-VEGF injections.
For dry AMD, currently, there is no specific treatment available. However, a special blend of vitamins, known as AREDS supplements, is recommended to help reduce the risk of progression of the disease.
Regular monitoring and management by retina specialist is crucial for both types of AMD to preserve vision and prevent further deterioration.
Intravitreal Injection
A course of several injections is typically recommended based on the specific macular disease diagnosed by the retina specialist. Each injection is administered approximately one month apart.
The procedure is conducted in a sterile environment to minimize the risk of infection. Before the injection, the eye is thoroughly cleaned, and local anaesthetic drops are administered to numb the eye. This helps ensure patient comfort during the procedure.

Retinal Detachment Surgery
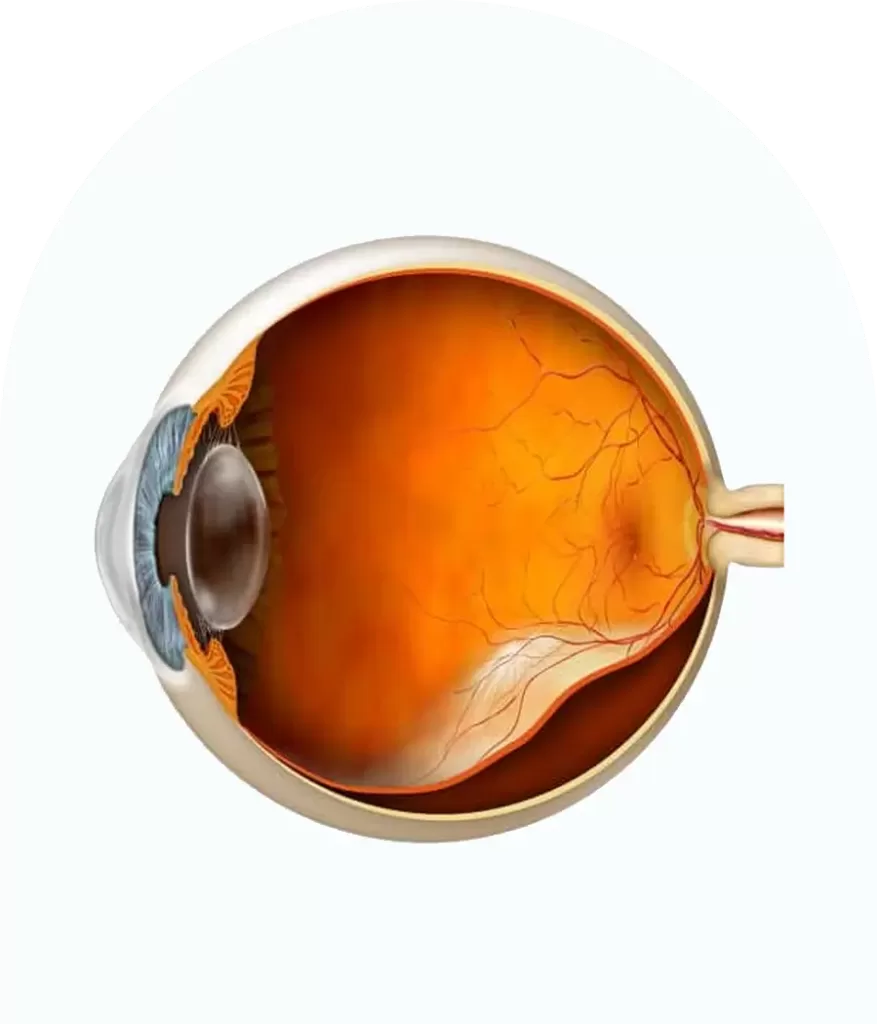
Retinal detachment occurs when the thin lining at the back of the eye, known as the retina, begins to pull away and separate from the underlying wall of the eye. This separation can disrupt the blood vessels that supply the retina with essential oxygen and nutrients. If not treated promptly, retinal detachment can lead to blindness in the affected eye.
The most common type of retinal detachment is called rhegmatogenous retinal detachment, which is typically caused by a tear or hole in the retina. Prompt surgical intervention is often necessary to repair this type of detachment.
There are other types of retinal detachment as well:
- Traction retinal detachment, often seen in advanced diabetic retinopathy, where scar tissue pulls the retina away from its normal position.
- Exudative retinal detachment, usually associated with conditions causing inflammation in the eye, leading to fluid accumulation under the retina.
Each type of retinal detachment requires specific management tailored to the underlying cause. Rhegmatogenous retinal detachment, in particular, usually necessitates urgent surgery to prevent permanent vision loss. Early detection and treatment are critical in preserving vision and preventing complications.
Treatment
Urgent treatment for retinal detachment is crucial to reduce the risk of permanent vision loss. The primary treatment for retinal detachment is surgical intervention; eye drops or medications alone are not effective for reattaching the retina.
Most cases of detached retinas can be successfully reattached through various surgical techniques. However, after surgery, there is typically a recovery period of several months during which vision may be weak. This can impact daily activities such as driving.
It’s important to note that some individuals may not regain full vision even after successful reattachment of the retina. Permanent reductions in peripheral (side) or central vision can occur in some cases, regardless of the success of the surgical procedure. The risk of permanent vision impairment is higher the longer the detachment remains untreated.
Early detection and prompt surgical treatment significantly improve the chances of restoring vision and minimizing long-term vision loss in cases of retinal detachment. Regular eye exams and immediate medical attention for symptoms such as flashes of light or sudden onset of floaters are essential for timely diagnosis and treatment.
