Symptoms
Symptoms experienced depend on the cause of the problem. These may include:
- Pain
- Redness
- Light sensitivity
- Doubling of vision
- Hazy vision
Examination / Diagnosis
The cornea’s abnormalities and subsequent diagnosis can be diagnosed by several tools like corneal topography, anterior OCT, specular microscopy and slit lamp examination.
If you experience any symptoms related to the cornea or require a comprehensive evaluation, we recommend scheduling an appointment with our skilled cornea specialist at Roya Eye Clinic who has undergone extensive subspecialty training in the field and are dedicated to diagnosing and treating various corneal conditions to ensure optimal eye health and vision for our patients.

The cornea, known as the clear window at the front of the eye, plays a vital role in vision. It provides two-thirds of the eye’s focusing power and is crucial for maintaining a clear and sharp image. However, the cornea can be affected by various conditions, including inflammatory diseases, infections, and shape disorders.
Some commonly seen corneal conditions include:
- Keratitis: Infection/inflammation of the cornea.
- Corneal abrasion: a scratch on the cornea occurring due to trauma or weakness of the epithelium (the outermost skin of the cornea)
- Corneal foreign body: a piece of debris embedding itself superficially on the surface of the cornea.
- Corneal laceration: a partial or full-thickness wound of the cornea as a result of trauma.
- Keratoconus: a condition causing thinning and distortion of the cornea
- Corneal scarring: As a result of trauma or previous inflammation of the cornea.
- Corneal dystrophies: inherited conditions causing gradual opacification of the cornea as a result of the metabolic by-products


Keratoconus
Keratoconus (KC) is a disorder of the eye that results in progressive thinning of the cornea. This may result in blurry vision, double vision, nearsightedness, irregular astigmatism, and light sensitivity leading to poor quality-of-life. Usually both eyes are affected. In more severe cases a scarring or a circle may be seen within the cornea.
While the cause is unknown, it is believed to occur due to a combination of genetic, environmental, and hormonal factors. Patients with a parent, sibling, or child who has keratoconus have 15 to 67 times higher risk in developing corneal ectasia compared to patients with no affected relatives. Proposed environmental factors include rubbing the eyes and allergies. The underlying mechanism involves changes of the cornea to a cone shape. Diagnosis is most often by topography. Topography measures the curvature of the cornea and creates a coloured “map” of the cornea. Keratoconus causes very distinctive changes in the appearance of these maps, which allows doctors to make the diagnosis.
Causes
Keratoconus has multiple causes, resulting in a cornea that is more elastic than normal and begins to thin and bulge forward, leading to reduced vision and increased astigmatism. It can be inherited, with a chromosomal link identified. Keratoconus is also associated with allergic diseases such as hay fever, eczema, and asthma, though it typically develops around puberty and is strongly linked to eye rubbing, which can accelerate its progression. Contact lens wearers are also at higher risk.
Early detection of Keratoconus is crucial for optimal outcomes, achievable through corneal topography. If left untreated, Keratoconus can result in significant visual impairment and potentially blindness.
Symptoms
- blurry and distorted vision
- increased near-sightednessor astigmatism (when your eye cannot focus as well as it should
- Not being able to wear contact lenses. They may no longer fit properly and they are uncomfortable


Non-surgical Treatment
- Spectacles: These can provide good vision in the early stages of the condition and usually help to correct myopic astigmatism.
- Hard or Scleral Contact Lenses: When spectacles don’t work, rigid contact lenses and Scleral lenses usually provide very good vision if the patient can tolerate them; they should be fitted by a contact lens specialist.
Surgical Treatment
- CXL – Corneal Collagen Cross-linking with Riboflavin (Vitamin B2): This technique strengthens the cornea and halts the progression of Keratoconus.
- Intracorneal Rings: These rings, inserted into the cornea, reshape the corneal cone, flattening it to a more regular shape and central position. This procedure improves vision in many patients who cannot tolerate contact lenses and have clear corneas with less advanced Keratoconus. A Femto-second laser creates tunnels and entry points for the rings, ensuring a safe and reliable procedure.
- Toric Implantable Contact Lenses: For stable Keratoconus with good vision using glasses, Toric Implantable Contact Lenses are often used after stabilizing the condition with corneal cross-linking. These lenses can eliminate the need for optical aids and improve vision balance between both eyes.
- Phototherapeutic Keratectomy (PTK): While Keratoconus patients are not candidates for LASIK or standard laser correction, some benefit from limited excimer laser treatment to improve corneal surface irregularities when contact lenses cannot be tolerated. PTK is typically combined with corneal cross-linking either during the same procedure or afterward.
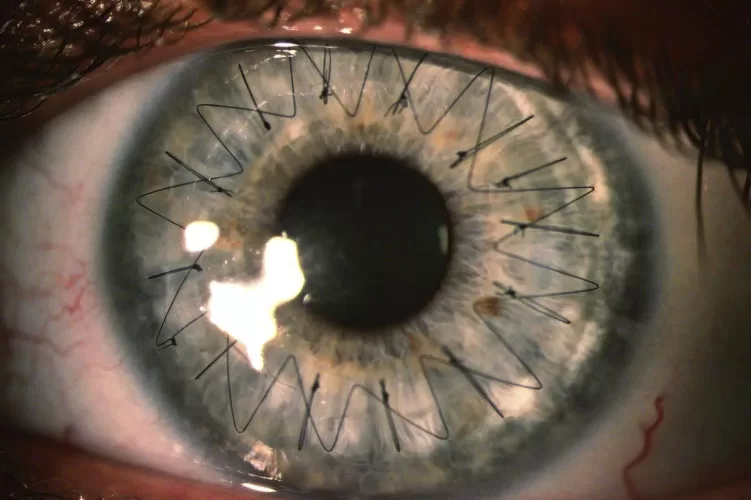
- Corneal Transplants: Reserved for advanced Keratoconus stages, corneal transplants include partial thickness (Deep Anterior Lamellar Keratoplasty = DALK) or full thickness grafts (Penetrating Keratoplasty = PK). However, the need for these procedures is declining due to improved early diagnosis of Keratoconus and the effectiveness of corneal cross-linking in stabilizing the condition, preventing it from reaching advanced stages in most cases.
Corneal Transplant
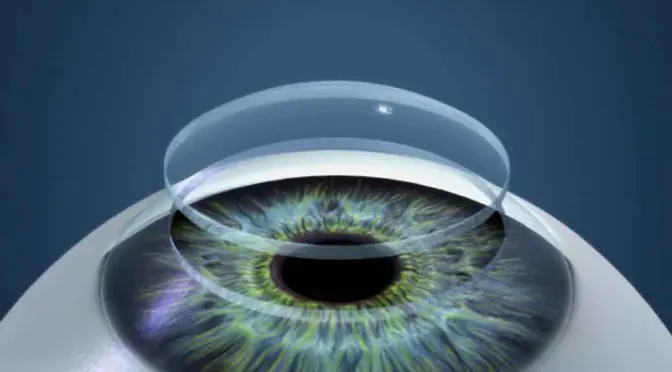
The cornea is a transparent tissue window at the front of the eyeball, allowing light to enter and providing focus for clear vision. Diseases or injuries can cause the cornea to become cloudy or change shape, disrupting the normal passage of light into the eye and impairing vision.
The cornea consists of three primary layers: thin outer and inner layers, with a thick middle layer. Certain conditions may affect only the innermost layer (endothelium), leading to corneal edema (swelling) and cloudiness.
Types of Corneal Transplants:
- Deep Anterior Lamellar Keratoplasty (DALK)
- Endothelial Keratoplasty (DSAEK and DMEK)
- Penetrating Keratoplasty
Deep Anterior Lamellar Keratoplasty (DALK)
Deep Anterior Lamellar Keratoplasty (DALK) involves removing the outer layers of the cornea and replacing them with donor tissue, resulting in a partial-thickness corneal transplant. The procedure typically involves using sutures, which are generally removed about a year after surgery.
Approximately 90% of patients achieve a vision good enough for driving, though glasses or contact lenses may still be necessary for optimal vision. In some cases, additional surgeries may be required.
Astigmatism is common after DALK and may require correction with glasses, contact lenses, or through further surgical interventions such as laser vision correction or implantation of a phakic intraocular lens after all sutures are removed.
Endothelial Keratoplasty (DSAEK and DMEK)
Endothelial Keratoplasty (EK) involves replacing the inside layer of the cornea with a donor layer, inserted through a small incision without the need for suturing the graft. This advanced procedure represents a newer type of corneal graft with significantly reduced complications.
Endothelial Keratoplasty offers faster recovery times compared to full-thickness grafts, primarily due to the smaller incision and the absence of suture-related issues such as astigmatism, broken sutures, or inflammation.
Penetrating Keratoplasty (PKP)
Penetrating Keratoplasty (PKP) involves a full-thickness transplant where all layers of the cornea are removed and replaced with a healthy corneal graft. Approximately 75% of patients achieve vision suitable for driving, though some may require vision aids or additional surgeries.
Risks associated with PKP are relatively uncommon but include corneal transplant rejection, graft failure, glaucoma, cataract formation, and high astigmatism.
All corneal transplant procedures are typically performed under either general or local anaesthesia and generally take about one hour to complete. Patients are usually discharged on the same day after surgery and require the use of steroid eye drops for about a year, or less for Endothelial Keratoplasty.

Corneal Cross-Linking
Corneal cross-linking (CXL) is a treatment for patients with keratoconus aimed at preventing the progression of their condition. Successful in more than 90% of cases, CXL halts the deterioration by strengthening the cornea. Keratoconus worsens as the cornea weakens, and CXL achieves this by using ultraviolet light and riboflavin (vitamin B2) drops to induce cross-linking of the corneal fibres. This process mimics the natural age-related hardening of the cornea, known as natural cross-linking.
Conditions associated
Keratoconus
Keratoconus is a progressive thinning of the cornea, the clear front window of the eye. Along with the intraocular lens, the cornea focuses light onto the retina. Normally, the cornea is a smooth, round, dome-shaped structure. However, in keratoconus, it becomes very thin and irregular, often protruding from the centre or below the centre like a cone. This irregularity causes blurry vision that is often not fully correctable with glasses alone.
CXL treatment
The treatment is recommended for patients whose scans indicate worsening keratoconus or who are at high risk, such as children. It is minimally invasive, involving local anaesthesia drops to ensure comfort during the procedure. Vitamin B2 (Riboflavin) drops are applied frequently for about 10-20 minutes then ultraviolet light is directed onto the cornea for about 10 minutes. This strengthens the cornea and can slow or halt the progression of the disease.
While the treatment aims to improve vision, glasses or contact lenses may still be necessary. In some cases, there may be slight improvement in keratoconus symptoms following treatment. Corneal cross-linking can also be combined with other procedures such as intracorneal ring implants or specific surface laser treatments either simultaneously or sequentially.
FAQ
Unlike conventional eye diseases, keratoconus is a chronic and lifelong condition that does not resolve on its own. Treatment options for keratoconus include collagen cross-linking, Toric phakic intraocular collamer lens implantation, intrastromal ring implantation, and in severe cases, corneal transplant. These interventions aim to manage the progression of the condition and improve visual outcomes for patients affected by keratoconus.
Depending on each patient’s specific needs, our keratoconus treatment protocol may include glasses, scleral contact lenses, other specialty contact lenses, and treatments for dry eyes. With the right combination of treatments, keratoconus patients can achieve 20/20 vision, addressing their visual challenges effectively.
The following may increase the risk of developing keratoconus:
- Patients with a family history of keratoconus or with certain systemic disorders, such as Down syndrome, are at a higher risk of developing keratoconus.
- Chronic eye inflammation. Constant inflammation from allergies or irritants can contribute to the destruction of corneal tissue that may result in developing keratoconus.
- Eye rubbing. Chronic eye rubbing is associated with developing keratoconus. It may also be a risk factor for disease progression.
- Keratoconus is often discovered in the teenage years. Generally, young patients with advanced keratoconus are more likely to need some form of surgical intervention as the disease progresses.
Many keratoconus patients are unaware they have the disease. The earliest symptom is a slight blurring of vision or progressively poor vision that is not easily corrected.
Other symptoms of keratoconus include:
- Glare and halos around lights
- Difficulty seeing at night
- Eye irritation or headaches associated with eye pain
- Increased sensitivity to bright light
- Sudden worsening or clouding of vision
