Cataract
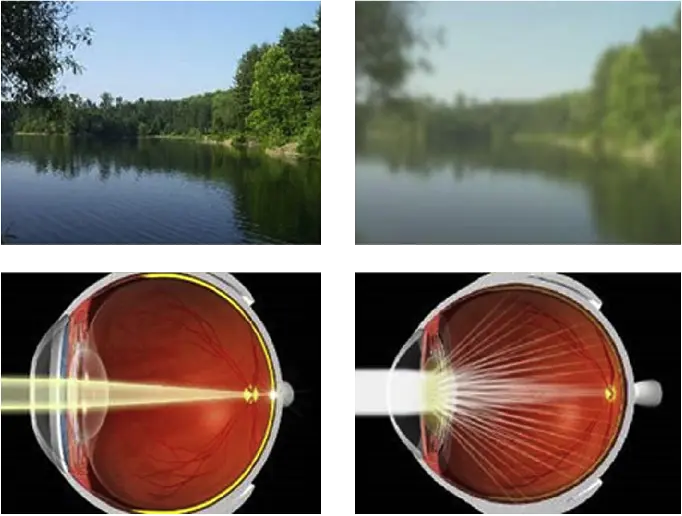
A cataract is a cloudy area in the lens of the eye that leads to a decrease in vision of the eye. Cataracts often develop slowly and can affect one or both eyes. Symptoms may include faded colours, blurry or double vision, halos around light, trouble with bright lights, and difficulty seeing at night. This may result in trouble driving, reading, or recognizing faces. Poor vision caused by cataracts may also result in an increased risk of falling and depression. Cataracts cause 51% of all cases of blindness and 33% of visual impairment worldwide.
Causes
Age is the most common cause of cataracts and most people will develop cataracts as they grow older. Other causes of cataracts or the development of cataracts at an earlier age include medical conditions like diabetes, certain medications like corticosteroids, high myopia, previous eye surgery, trauma etc.
Conditions associated
- Diabetes mellitus
- Previous eye surgery
- Previous trauma to the eye
- Familial cataract
Symptoms
Symptoms for cataracts include blurring of vision, difficulty in contrast, especially shades of colours, frequent change in the glass’s prescription, glare or light scatter
Cataract Surgery
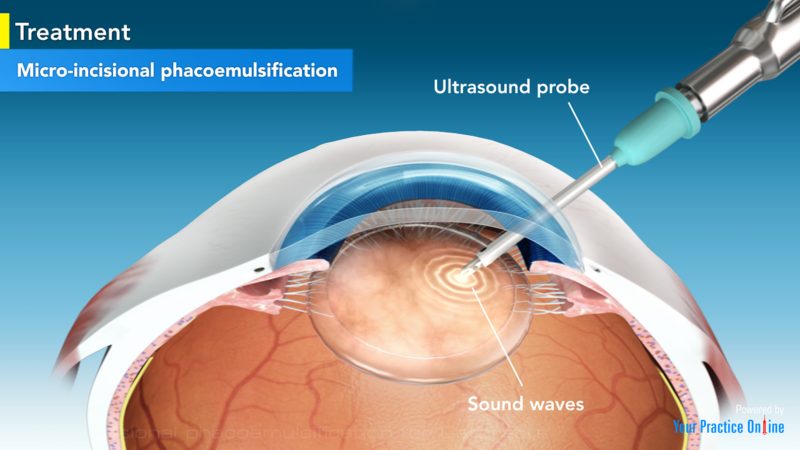
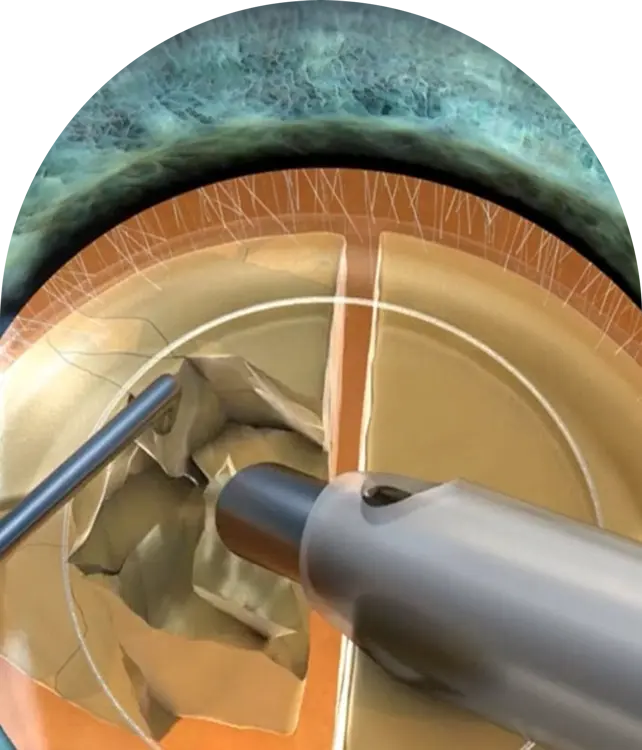
Phacoemulsification is a cataract surgery method in which the internal lens of the eye which has developed a cataract is emulsified with the tip of an ultrasonic handpiece and aspirated from the eye. Aspirated fluids are replaced with irrigation of balanced salt solution to maintain the volume of the anterior chamber during the procedure. This procedure minimises the incision size and reduces the recovery time and risk of surgery-induced astigmatism.
It is suited to all types of cataracts, where the ultrasonic energy required is mild, moderate and high depending on the cataract density, and insertion of foldable intraocular prosthetic lenses, which take advantage of the small incision possible. It is the most common procedure for cataract removal in the developed world, with an excellent prognosis in uncomplicated cases.
Preparation and precautions
Anaesthesia
Proper anesthesia is essential for ocular surgery. A facial nerve block may occasionally be performed to reduce lid squeezing. General anesthesia is recommended for children, traumatic eye injuries with cataract, for very apprehensive or uncooperative patients and animals. Cardiovascular monitoring is preferable in local anesthesia and is mandatory with general anesthesia.
Either topical, sub-tenon, peribulbar, or retrobulbar local anaesthesia is used, usually causing the patient little or no discomfort. Topical anaesthetics are most commonly used; these are placed on the globe of the eye as eyedrops before surgery or in the globe during surgery. Local-anaesthetic injection techniques include sub-conjunctival injections and injections behind the globe (retrobulbar block) to block regional nerves and prevent eye movement. Intravenous sedation may be combined with the local anaesthetic.
Site preparation
Proper sterile precautions are taken to prepare the area for surgery, including use of antiseptics like povidone-iodine. Sterile drapes, gowns and gloves are employed. A plastic sheet with a receptacle helps collect the fluids during phacoemulsification. An eye speculum is inserted to keep the eyelids open. The operation site is prepared by disinfection of the area around the eye and any other exposed area of the face, and exposure of the eyeball using an eyelid speculum.
Recovery and rehabilitation
Following cataract surgery, side-effects such as grittiness, watering, blurred vision, double vision or a red or bloodshot eye may occur, and will usually clear after a few days. Full recovery can take four-to-six weeks. Patients are usually advised to avoid getting water in the eye during the first week after surgery, and to avoid swimming for two-to-three weeks as a conservative approach, to minimise risk of bacterial infection. Most patients can return to normal activities the day after phacoemulsification surgery.] Patients should avoid driving for at least 24 hours after the surgery, largely due to possible swelling affecting focus, and pupil dilation causing excessive glare. At the first post-operative
check, the surgeon will usually assess whether vision is suitable for driving.
With small-incision self-sealing wounds used with phacoemulsification, some of the post-operative restrictions common with intracapsular and extracapsular procedures are not relevant. Restrictions against lifting and bending were intended to reduce the risk of the wound opening, because straining increases intraocular pressure. With a self-sealing tunnel incision, however, higher pressure closes the wound more tightly. Routine use of a shield is not usually required because inadvertent finger pressure on the eye should not open a correctly structured incision, which should only open to point pressure. After surgery, to prevent contamination, the eyes should not be rubbed and the use of eye makeup, face cream or lotions should be avoided. Excessive dust, wind, pollen or dirt should also be avoided. Sunglasses should be worn on bright days because the eyes will be more sensitive to bright light for a while.
Topical anti-inflammatory drugs and antibiotics are commonly used in the form of eye-drops to reduce the risk of inflammation and infection. A shield or eye-patch may be prescribed to protect the eye while sleeping. The eye will be checked to ensure the IOL remains in place, and once it has fully stabilised, after about six weeks, vision tests will be used to check whether prescription lenses are needed. Where the focal length of the IOL is optimised for distance vision, reading glasses will generally be needed for near focus.
Outcomes
After full recovery, visual acuity depends on the underlying condition of the eye, the choice of IOL, and any long-term complications associated with the surgery. More than 90% of operations are successful in restoring useful vision, with a low complication rate. The World Health Organization (WHO) recommends at least 80% of eyes should have a presenting visual acuity of 6/6 to 6/18 (20/20 to 20/60) after surgery, which is considered a good visual outcome, and that with best correction this should be at least 90%. Acuity of between 6/18 and 6/60 (20/60 to 20/200) is regarded as borderline, and worse than 6/60 (20/200) is considered poor. Borderline or poor visual outcomes are usually due to pre-surgery conditions such as glaucoma, macular disease, and diabetic retinopathy.
FAQ
The cataract surgical procedure is completely safe, and you don’t feel any pain. Eye care specialists at Roya Eye Clinic take preventive measures and perform this surgery using advanced tools and techniques.
Any eye problem, if left untreated, causes vision difficulty or loss later. If you don’t treat cataracts on time, it may get worse with time, causing blindness. If you wait for too long, cataracts can become hyper-mature. This causes complications in eye cataract operation, so you must consult our doctors at the right time for hyper-mature cataract treatment.
The lens where the cataract develops has been removed and replaced, so there is no possibility of the cataract growing back. An intraocular lens (IOL) implant does not require maintenance or replacement.
To help you understand how cataracts are diagnosed, our doctors perform multiple cataract eye tests, such as retinal examination, visual acuity test, and slit-lamp test. Based on these procedures, they recommend cataract surgery if needed. To restore your vision, doctors use intraocular lenses for cataract surgery.
